|
|
|

THE BIG DIFFERENCE IN EHR /
EMR
Accuracy ─ Efficiency ─
Compliance
Electronic
Medical Records Review and Audit
─
What We Offer
─
Objectives
─
Report Set #1 & Set #2
▀
WHAT WE OFFER
The Electronic Medical Records review
process has the objective to thoroughly audit the electronic collection
of facility-generated health information. This audit is conducted
according to the set standards of nursing principles and practices. Our
friendly review specialists have extensive experience with most commonly used EHR/EMR
reporting software
applications like PCC (PointClickCare), Matrix, etc.
During this process we identify deficiencies,
discrepancies and any concerns regarding the applicable documentation
which must be reported to respective key personnel for modification,
refinement and/or further supplementation. Based on our audits, our
review specialists will be able to provide suggestions on how to improve
a facility's percentage per QM (Quality Measure).
Accurate documentation is essential of
communicating each patient's current condition to the health care team.
This is the basis for patient-centered health care plans. Due to its
significance, it is very important to maintain a faultless medical
record. To ensure precise, complete and accurate health records, each
specialist must:
|
▀ |
Check and
keep track of PASRR completion upon admission and renewal. |
|
▀ |
Analyze PASRR level 1 evaluation and
identify the need for level 2. |
|
▀ |
Maintain an updated record of
completed baseline care plans and report due accomplishment 48 hours
after admission. |
|
▀ |
Keep track of daily census actions
and report completion status of required documents as stated in
federal regulations and nursing principles. |
|
▀ |
Ensure that necessary details are encoded
and made available on patientís health records as demanded by patientís
current health status reflected in the system.
|
|
▀ |
Determine incidents of events and
sustained injury by reviewing created progress notes, assessment forms and care plans, and
inspect if vital details are rightfully documented and if proper notification was observed.
|
|
▀ |
Monitor medical records of patients
receiving skilled services and tracks daily skilled documentation.
|
|
▀ |
Thoroughly examines completed progress
notes and assessment forms to identify issues and concerns due for modification, refinement
and supplementation.
|
|
▀ |
Update a tracking sheet for essential
assessments and care plans as mentioned in various regulations and ensure completion upon
admission and as per renewal schedule.
|
|
▀ |
Records cases of infection and streamline
tracking sheets as to management and infection control measures taken.
|
|
▀ |
Surveys medication orders to ensure its
appropriateness on the indication and the sufficiency of provided order details.
|
|
▀ |
Surveys psychotropic medication
orders and audits incompleteness of supplementary documentation
demanded to ensure residentís safety and the managementís
effectiveness. |
|
▀ |
Identify gradual dose reduction
schedule of psychotropic medications and record attempts of
tapering, until discontinued. |
|
▀ |
Note new pressure-related skin
conditions and check weekly skin assessment until resolved. |
|
▀ |
Scrutinize implemented actions for
different health issues and evaluate its appropriateness and
effectiveness. |
|
▀ |
Identify areas of improvement that
could enhance evaluation of quality measures of the facility. |
|
▀ |
Reports and coordinates findings and
urgent concerns with facility key persons for deliberation of
actions to be taken. |
▀
OBJECTIVES
|
▀ |
To maintain precise and
comprehensive health records as determined by patientís present medical conditions in accordance to set regulations and
standards. |
|
▀ |
To identify
documentation issues due for modification, refinement or further supplementation. |
|
▀ |
To raise facility
ratings and improve survey outcomes. |
|
▀ |
To ensure the retrieval
of accurate and complete facts from the patientís record by authorized members of the health care team in
establishing good and effective health
management plans. |
▀
REPORT SET #1 & SET #2
─
Set #1 Report Detail
─
Set #2 Report Detail
|
SET #1 |
|
SET #2 |
|
Report |
Review and Reporting Schedule |
Report |
Review and Reporting Schedule |
|
PASRR & Baseline Care
Plan |
Daily |
Antibiotics |
Daily |
| Discharge |
Daily |
Blood Thinners |
Weekly |
| Daily Medicare
Charting |
Daily |
Pressure Ulcers |
Weekly |
| Incidents |
Daily |
Psychotropics |
q15 days |
| Change of Conditions |
Daily |
Falls |
Monthly |
| Admission |
14 days after
admission |
|
| Quarterly and Annual
Assessments |
Weekly |
▀
SET #1
1.
PASRR & Baseline Care Plan
2.
Discharge
3.
Daily Medicare Charting
4.
Facility Reported Incidents
5.
Change of Conditions
6.
Admissions
7.
Assessments
1. PASRR & Baseline Care Plan
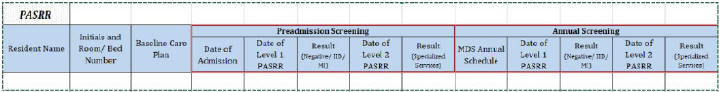
Click to Enlarge
|
This template is based on reviewed PASRR
regulations (ß483.106, 42 CFR ß 483.20, ß483.104, ß483.104). It is intended to cover all
screening due upon admission to facility. Further, this template is also
provided for PASRR renewal, reflecting
evaluation results to determine the need for PASRR Level 2.
The review is an easy
reference for all completed forms as well as those whose preadmission screening file is not
yet available in the system. PASRR is vital in determining the level of care
required by a residentís
condition and is also very important in billing matters. By providing our client daily
with updated
review findings, it will be easier to achieve 100% compliance.
|
2. Discharge
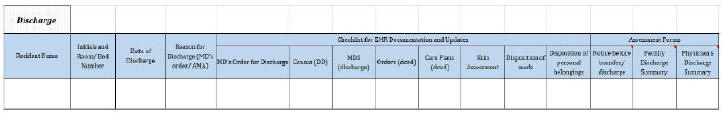
Click to Enlarge
|
This template is based on standards for
discharges from nursing facilities. All discharged residents will be
listed and important updates in census, MDS and care plans will be
reviewed. This will prevent loss of pertaining data at future
facilities. In addition, key assessments and documentation upon
discharge will be covered in this review to prevent future conflicts.
The regulations state the required forms
and details that are essential when a patient is leaving the facility
and the time allowed to complete the pertaining forms. Clinical review
specialists will make sure that all missed chartings will be reported
and followed-up by the facility to achieve comprehensive and precise
documentation.
|
3. Daily Medicare
Charting
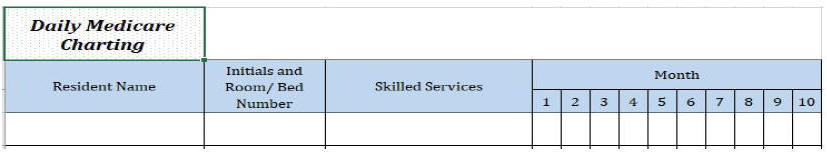
|
This review will cover all active
Medicare residents in the facility. Daily reports of Medicare charting
due and any concerns (e.g. missed charting, skilled services not
reflected) will be provided to the facility for easy citing and
timely improvement.
In this tracking log, active skilled
services of the listed resident will be reflected and for the facility's
reference the resident's remaining Medicare days are reported.
Therefore, it is possible to achieve 100% compliance.
|
4.
Facility Reported Incidents
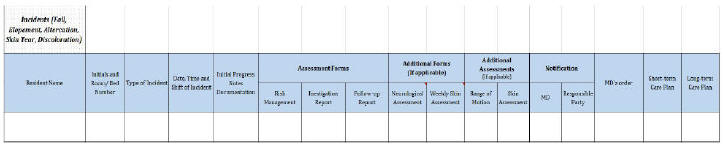
Click to Enlarge
|
By providing the client a detailed
table for each event, the facility will have a comprehensive
overview of the incidents as well as the status of the files which
are required for each and every occurrence. This will boost
acceptance and compliance for the specifications set by federal,
state and local authorities.
Most importantly, it will allow the
facility to evaluate effectiveness of existing interventions and
implement client-centered approaches to prevent future cases. |
5. Change of
Conditions
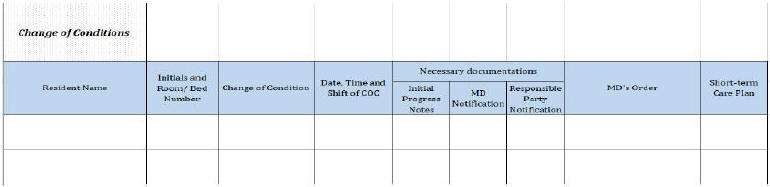
Click to Enlarge
|
This review is providing the client
a list of change of condition cases and findings after a
comprehensive review of available data in the system. This is also
a guide for medical records reviewer on what to check for in
making certain that proper assessment was completed.
In addition, licensed physicians
are able to view at a glance that they were made aware of
essential actions, and that care planning is initiated and
maintained for each resident's fast recovery. |
6. Admissions
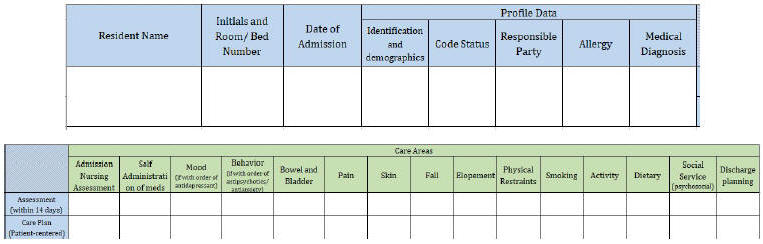
Click to Enlarge
|
This report provides tracking of
new admissions together with a checklist for required resident
information, including assessment findings required by pertaining
regulations. In this review, various care areas are covered to
warrant their availability for assessment forms and care planning.
This template is providing ease of
completion for an extensive and multidisciplinary evaluation to
the client in order to save the client substantial time. |
7. Assessments
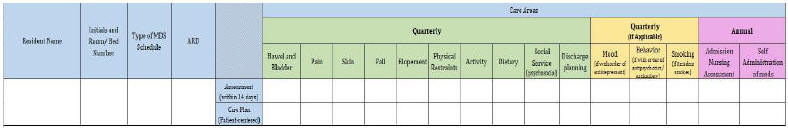
Click to Enlarge
|
We carefully studied the
regulations pertaining to assessments in order to provide a
thorough template. Particular attention was given to the
recommended schedule of renewal to ensure constructive timing for
the betterment of all patients and adherence to the standards.
This tracking sheet is a great tool
to accurately complete the required forms despite the many
challenges to perform this task correctly. Included in this review
are the assessments required upon admission which were arranged
according to their renewal timetable based on the MDS scheduler.
The review specialist will identify
residents who were due to be assessed in the previous week. The
findings will be forwarded to key personnel on a weekly basis. All
number of days will be calculated from the ARD of each scheduled
MDS assessment due. |
▀
SET #2
1.
Antibiotic and Infection Review
2.
Blood Thinners
3.
Pressure Ulcers
4.
Psychotropics
5.
Fall Incidents
1. Antibiotic and Infection Review
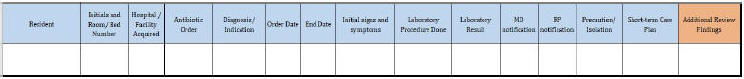
Click to Enlarge
|
This template's purpose is to track
residents with antibiotic orders to easily identify
possible/actual outbreak in the nursing facility. In addition, the
study will provide every condition to be comprehensively reviewed
to determine that details are completed and rightfully documented.
Otherwise, modifications for
improvements and further supplementations will immediately be
completed. CFR has also enumerated vital information to be noted
and actions to be taken which is the basis for this template. |
2 .
Blood Thinners
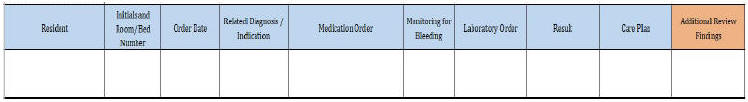
Click to Enlarge
|
This review is intended to track
all active blood thinners and perform weekly updates, especially
for those medications that need laboratory orders to ensure
rightful dosage. Also reflected in this log is the review of
documentations for bleeding monitoring both in care plan and
order. Having the monitoring order with precise scheduling
details, the system will remind nurses to always watch out for
signs of this alarming side effects.
Necessary files like care plan and
appropriateness of indication/related diagnosis indicated in the
order will be double checked. In such a case, with this review we
not only improve nursing documentations and compliance to
standards, but we also guarantee quality and effective care. |
3. Pressure Ulcers
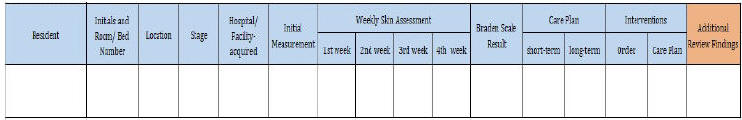
Click to Enlarge
|
This review is providing the
facility an in-depth review of each pressure sore case. It
indicates if necessary details as suggested by regulations are
provided in the electronic medical records, preventing citations.
Weekly assessment of each skin condition noted will also be
tracked to determine if ulcer is improving or worsening.
This will evaluate if current the
management plan is effective or is in need improvement. Active
interventions will be indicated in this tracking sheet. Therefore,
it is easy to determine its appropriateness, effectiveness and
consistency in the health records. |
4. Psychotropics
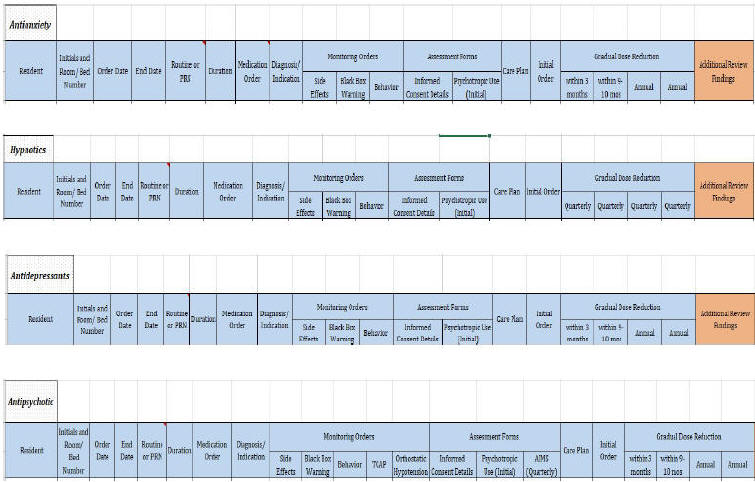
Click to Enlarge
|
By accomplishing and maintaining
these tracking sheets, we will easily track medication orders to
implement immediate action. The following are the common findings
that we note upon review:
(i) diagnosis doesnít match the
mechanism of action of medication;
(ii) manifested behavior doesnít match the diagnosis;
(iii) manifested behavior is too broad and needs to be specified;
(iv) dose and frequency indicated might exceed the maximum
administration dosage for 24 hours;
(v) prn order might exceed 14 days;
(vi) might not contain vital information.
In addition, this review has the
objective to ensure that monitoring of possible side/adverse
effects is maintained, and vital forms are completed.
Tracking of gradual dose reduction
as per each medication classification schedule will also be
indicated in this log. Due gdr evaluation will be reported to
facility as scheduled. |
5. Fall Incidents
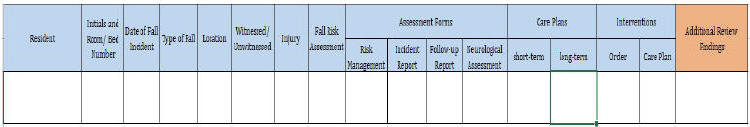
Click to Enlarge
|
This template is to provide client
a comprehensive list of fall incidents and information about the
occurrence. By recording those, we will make sure that complete
data was provided regarding each fall incident. Each residentís
risk of falling will also be reflected in this sheet to determine
if it is updated with the residentís current condition or needs to
be reevaluated.
Short-term care plan for every fall
incident will also be tracked and recorded as well as the
long-term care plan for every high-risk resident. |
▀
ABOUT US
At Scherf Health, our focus is to provide
superior EHR/EMR review and audit services for Nursing Home facilities
and Assisted Living facilities throughout the U.S.
Scherf
Health
is part of Scherf Corporation which was
established in the U.S. in 1990. Since 1996, we've been based in Las
Vegas, Nevada.
The
Scherf
Health staff is comprised of a team
of top professionals who have many years of experience in this specific
field of service. Our friendly review specialists receive constantly compliments
from our very satisfied clients regarding our invaluable services.
Depending on size and number of facilities, for each client we'll put
together a team. Specifically assigned members
of the team will be available to your DONs and pertaining facility staff
for assistance with the EHR/EMR reviews/reports by Email (24/7) and by telephone
(during regular business hours).
At
Scherf
Health, we have full confidence in
the highest quality of our services and the best offering in the U.S.
Highly competitive pricing with flexible month-to-month service
contracts make
Scherf
Health the #1 choice for all your
review and audit needs to achieve superior compliance and help improve
ratings and CMS averages. We also offer
flexibility as you can add and remove facilities with ease. If you're
not fully satisfied with our services or for any other reason, you may
cancel at any time, no strings attached.
Sign up today or
contact us for any questions that you
may have.
Kindly,
Dietmar Scherf
CEO & President
Scherf Corporation
|

|
|